ADVERTISEMENT
Evacuate or Shelter in Place? Prepare Ahead for a Critical Decision
ECRI Institute and Annals of Long-Term Care: Clinical Care and Aging (ALTC) have joined in collaboration to bring ALTC readers periodic articles on topics in risk management, quality assurance and performance improvement (QAPI), and safety for persons served throughout the aging services continuum. ECRI Institute is an independent, trusted authority on the medical practices and products that provide the safest, most cost-effective care.
Events that may force health care facilities to make decisions about evacuating or sheltering in place are becoming more common.1 Because internal or external situations may require either partial or total evacuation, health care organizations should assess their organization’s risks, devise a comprehensive evacuation plan, and test the plan. The plan should incorporate strategies to conduct planned and unscheduled evacuations.
Unless directed by government mandate, health care facilities have the authority to determine whether and when it is in their patients’ best interests to evacuate or shelter in place. Unfortunately, major disasters continue to occur, yet they provide lessons learned and offer opportunities for facilities to learn how to better prepare for an evacuation.
This article will discuss how aging services facilities can determine whether to evacuate or shelter in place, types of evacuations, and relevant guidance and regulations to consider.
The Need to Evacuate
Many events could force a facility to evacuate some or all of its patients. Before Hurricane Katrina in 2005, some health care facilities never considered evacuation in the face of external disasters. Instead, the focus was on sheltering in place (also called defending in place). Many organizations were confident their disaster mitigation plans and backup systems would prevent them from being seriously impacted by disaster. However, experience has shown that health care organizations continue to “fail to incorporate even basic components into their evacuation plans, such as contingency planning for critical supplies, or ways to evacuate patients off-site.”2 The Centers for Medicare & Medicaid Services (CMS) responded by enacting the emergency preparedness rule.3 Now, health care facilities, like other businesses, are required by federal, and often state, law to have evacuation plans in response to the hazards identified by an all-hazard risk analysis.
CMS’ 2016 emergency preparedness rule explicitly addresses evacuation three times.4 The rule requires as follows:
- Providers must have policies and procedures that address safe evacuation.
- Providers must make arrangements with other organizations to ensure continuity of care.
- No facility is immune to a situation that may force an evacuation, and all organizations should be prepared to handle not only the potential event but also the serious and delicate operation of evacuating patients to safer facilities when needed.
Types of Evacuations
There are different types of evacuations dependent on context. An isolated fire or loss of power in one part of the facility might not necessarily require the entire facility to be evacuated. Risk managers should become familiar with the following definitions related to evacuations5:
- Horizontal evacuation: Movement of patients and staff to a safer area on the same floor (close to an emergency exit, if possible).
- Vertical evacuation: Movement of patients and staff to a safer area on a different floor.
- Partial evacuation: Movement of certain groups of patients or people in certain areas of the facility.
- Complete evacuation: Evacuation of the entire facility.
The time required to prepare for an event will have an effect on the evacuation decision and type. Some events, such as a fire, will require an immediate evacuation from the affected area. A hurricane, however, usually provides time to prepare for a possible evacuation. Organizations should determine the language they will use to describe evacuation time frames. One set of recommended terms is as follows5:
- Immediate/emergent: These events allow little or no time for preparation. Patients and others must be evacuated immediately.
- Rapid/urgent: These events allow a limited time to plan and prepare. Everyone is evacuated within 4 to 6 hours.
- Gradual/planned: These events allow for an extended period to plan and execute the evacuation. Evacuation could happen in phases over many hours or days.
- Prepare only: The facility is preparing for a potential evacuation, and no patients are moved.
Weighing the Risks and Benefits of Evacuation
The decision to evacuate patients is not easy. Risks are inherent in moving many individuals from one health care facility to another (eg, emotional trauma, physical injury, medical error). For nursing homes in particular, the mass movement of persons during an emergency event—persons who are often extremely frail, bed-ridden, comatose, cognitively impaired, and/or dependent upon ventilators or intravenous feeding or hydration equipment—has considerable health implications.6 If, however, a facility is not safe for patients or staff, evacuation is necessary.
Several factors can influence the effectiveness of an evacuation, including an organization’s “size, geographic location, physical layout, setting (ie, urban vs rural), and patient makeup, combined with the reason for evacuation.”2 Other considerations include legal issues, such as federal, state, and local laws, that are implicated during a disaster, such as the following7:
- Limitations in provider scope of practice (eg, physicians, nurse practitioners)
- Portability of practitioners’ licenses
- Credentialing of volunteer practitioners
- Immunity and liability concerns for volunteers
- Scope of waivers created by emergency declarations
Unfortunately, the decision to evacuate is not always clear. When there is time to decide, as in the case of an approaching hurricane, a decision must be made whether to shelter in place or to evacuate. However, the storm may change direction, missing the facility entirely. The decision to evacuate requires a comprehensive risk-benefit analysis, weighing inherent risks to the patients, including trauma vs risks that come from sheltering in place with potentially insufficient life-sustaining power, water, and staff and the inability to properly care for patients.
Sometimes, however, the decision to evacuate must be made quickly. In the 2018 California Camp wildfire, hospital nurses relayed harrowing stories of their experiences when quickly evacuating patients. The wildfire moved at an astonishing speed owing to high winds. One nurse attributed the successful rapid evacuation of all patients from the hospital (within 20 minutes) to the hospital’s emphasis on drills. However, once the patients were on their way to safety, the remaining staff were trapped by the wildfire; they nearly died trying to escape.8
Deciding to Evacuate vs Sheltering in Place
CMS does not specify factors organizations should consider when deciding between evacuating and sheltering in place, but it does require that such consideration take place and be documented.4 Sometimes, the only option may be to evacuate, but often deciding whether to evacuate or to shelter in place is not straightforward.
Factors to consider when determining whether to evacuate include the following9:
- Critical infrastructure vulnerabilities
- Power for life support equipment
- Ability to safely move patients to street level without elevators
- Transportation options that may not be available or routes that may be impassable after a storm
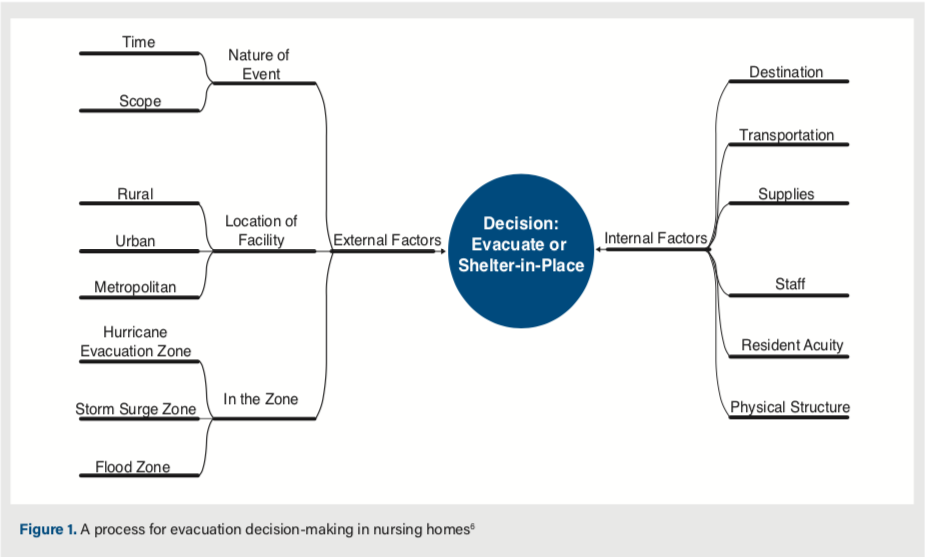
Factors influencing evacuation planning include weighing the risk of harm to patients; the likelihood for continuity of operations; prior experience with evacuation or shelter-in-place strategies; and cost (Figure 1). McGinty et al recommend collecting morbidity and mortality data for both evacuation and shelter-in-place strategies.10
The decision to evacuate or to shelter in place will implicate patient safety and satisfaction, along with financial and reputational risk. In a study examining the evacuation decision-making process, one study participant remarked that “the evacuation order is the hardest thing that we will ever have to do in our careers.” Other study participants perceived the evacuation decision as being a potentially “career-ending decision.” Either decision will likely be criticized: moving patients out of the facility if it turns out not to have been necessary or failing to evacuate if catastrophe strikes. Another concern is that, once a facility is evacuated and damaged in a disaster, it may not reopen.10
Researchers and those in the field point out that while many call for evacuation plans, guidance regarding the decision to evacuate is scarce. The Florida Health Care Education and Development Foundation released the National Criteria for Evacuation Decision-Making in Nursing Homes in 2008.6 The Agency for Healthcare Research and Quality published an evacuation decision guide in 2010, and an algorithm to help with evacuation decisions is also available.11
The National Fire Protection Association recommends the “RED” decision-making model, for “React, Evaluate, and Decide”12:
- Take any indication of smoke, fire, or other potentially threatening situation seriously (react).
- Determine the level of threat (evaluate).
- Make one of two decisions (decide):
- Follow the evacuation plan immediately
- Choose to defend in place (for instance, moving to the other side of a fireproof barrier, such as a fire wall, and taking protective or defensive actions, such as alerting the fire department to your location and sealing doors, windows, and vents)
In an actual disaster situation, incident commanders at the facility would have to consult with the community command structure to determine whether conditions in the area would support safe evacuation of patients and staff. It may be helpful to provide internal staff members with disaster management training that overlaps with the training received by outside disaster management organizations.
After Hurricane Katrina, Joint Commission standards were updated. EM.02.01.01 requires that an organization maintain systems to meet its own needs regarding communications, resources and assets, security and safety, staff, utilities, and patient care for at least 96 hours. The standard explicitly provides that organizations do not need to stockpile 96 hours’ worth of supplies, however. Having these resources, moreover, will not mean that all evacuations can be avoided.13 Planning cannot anticipate all needs; one organization used 96 hours’ worth of supplies in just over 4 hours during a disaster.14 Organizations should also consider whether medications are stocked in sufficient quantities for a prolonged shelter-in-place event, including medications needed personally by staff.
The community surrounding the health care facility may also be a factor in making the decision to evacuate. Civil unrest was noted in the days after Hurricane Katrina and became a factor leading some organizations to evacuate; however, civil unrest also prevented evacuation in some cases, for example, when ambulances traveling to pick up patients had to turn around because of security fears. Security is another factor to consider, as police and other municipal services may not be available to assist the facility in certain disaster situations if their help is urgently needed elsewhere. Facilities encountering security-related problems have reported hiring private companies to help.11 Enhanced safety and security measures may also be necessary to prevent looting and other dangers posed in affected areas.
Conclusion
Evacuating a medical facility is a costly and complicated process. A facility may not be able to plan for every potential emergency or evacuation scenario, but the basics of evacuation (eg, transporting patients, coordinating with government authorities and receiving facilities) will be similar, no matter the cause. Review common issues that can affect the decision to evacuate, such as the time it will take to evacuate, time of expected event impact, patient acuity, and building structure stability.
References
1. National Oceanic and Atmospheric Administration. Billion-dollar weather and climate disasters. ncdc.noaa. gov website. https://www.ncdc.noaa.gov/billions/. Accessed October 18, 2019.
2. Hicks J, Glick R. A meta-analysis of hospital evacuations: overcoming barriers to effective planning. J Healthc Risk Manag. 2015;34(3):26-36. doi:10.1002/jhrm.21162
3. 42 CFR § 482.15. Medicare condition of participation: emergency preparedness. https://www.law.cornell.edu/cfr/text/42/482.15. Accessed October 18, 2019.
4. Centers for Medicare & Medicaid Services (CMS). Survey and certification emergency preparedness initiative: S&C emergency preparedness checklist revision [memorandum]. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-12.pdf. Published February 28, 2014. Accessed October 18, 2019.
5. Massachusetts Department of Public Health (MDPH). Hospital evacuation toolkit. mass.gov website. https://www.mass.gov/lists/hospital-evacuation-toolkit. Published 2014. Accessed October 18, 2019.
6. Florida Health Care Education and Development Foundation. National Criteria for Evacuation Decision-Making in Nursing Homes. https://www.in.gov/isdh/files/NationalCriteriaEvacuationDecisionMaking.pdf. Published 2008. Accessed October 18, 2019.
7. Hershey TB, Van Nostrand E, Sood RK, Potter M. Legal considerations for health care practitioners after superstorm Sandy. Disaster Med Public Health Prep. 2016;10(3):518-524. doi:10.1017/dmp.2016.33
8. Rosenblatt K. Nurses fleeing fast-moving Camp Fire scramble to save patients—and themselves. NBC News. November 11, 2018. https://www.nbcnews.com/news/us-news/nurses-fleeing-fast-moving-camp-fire-scramble-save-patients-themselves-n934961. Accessed October 18, 2019.
9. Hassol A, Biddinger P, Zane R. Hospital evacuation decisions in emergency situations [letter]. JAMA. 2013;309(15):1585-1586. doi:10.1001/jama.2013.2470
10. McGinty MD, Burke TA, Resnick B, Barnett DJ, Smith KC, Rutkow L. Decision processes and determinants of hospital evacuation and shelter-in-place during Hurricane Sandy. J Public Health Manag Pract. 2017;23(1):29-36. doi:10.1097/PHH.0000000000000404
11. Zane R, Biddinger P, Hassol A, Rich T, Gerber J, DeAngelis J; Agency for Healthcare Research and Quality. Hospital evacuation decision guide. AHRQ pub. no. 10-0009. https://archive.ahrq.gov/prep/hospevacguide. Published May 2010. Accessed October 18, 2019.
12. National Fire Protection Association (NFPA). FAQs about building evacuation. https://www.nfpa.org/Public-Education/By-topic/Property-type-and-vehicles/High-rise-buildings/FAQs-about-building-evacuation. Accessed October 18, 2019.
13. Powell T, Hanfling D, Gostin LO. Emergency preparedness and public health: the lessons of Hurricane Sandy. JAMA. 2012;308(24):2569-2570. doi:10.1001/jama.2012.108940
14. South Dakota Department of Health. August 2, 2011 medical response to Joplin tornado May 22, 2011. https://doh.sd.gov/documents/Providers/Prepare/Joplin.pdf. Published August 2, 2011. Accessed October 18, 2019.










